Danger of Delirium
Delirium is among the most common of medical emergencies. It can occur in around 20% of adult acute general medical patients as well as:-
- In up to 50% of those who have a hip fracture.
- In up to 75% of those in intensive care.
Having dementia increases the risk of delirium. Other risk factors include: being aged 65 years or older, frailty, multiple illness, being male, have a history of depression, misuse of alcohol and experiencing sight or hearing loss.
Definition of Delirium and presentation
Delirium is defined as “an acute deterioration in mental functioning arising over hours or days that is triggered mainly by acute medical illness, surgery, trauma, or drugs” (SIGN 157). It may present as a state of sudden confusion or drowsiness that can happen when someone is unwell.
Delirium can be upsetting and frightening for the person experiencing it and for those around them. For this reason, it is really important that as many people as possible know about delirium so they can understand what’s happening and seek help as soon as delirium is suspected. The experience of delirium will be different for everyone but these are few examples:
| Feeling suspicious of others Being irritable, anxious or frightened Finding it hard to sit still Feeling agitated and restless Seeing things that aren’t there. | Not knowing where you are or why Being unable to keep up with conversations Feeling incredibly drowsy and slow Wanting to sleep all the time Showing no interest in eating or drinking |
Because of the many different ways delirium can present itself, it is often the people who know the person best who are first to notice. This is especially the case for people living with dementia, where subtle changes in a person’s activity levels or personality can provide valuable early warning signs (Delirium Part 2 below for further information).
Detecting Delirium
The “SQiD” or Single Question in Delirium is a simple but highly effective way of helping to detect delirium. Anyone can ask the SQiD and it can be used at home, in hospital or in a care home setting. Any time a person at risk of delirium is unwell:
SQiD = “Is the person more confused or drowsy today?”
If the answer is yes, it’s important to alert the persons GP or medical team that it might be delirium.
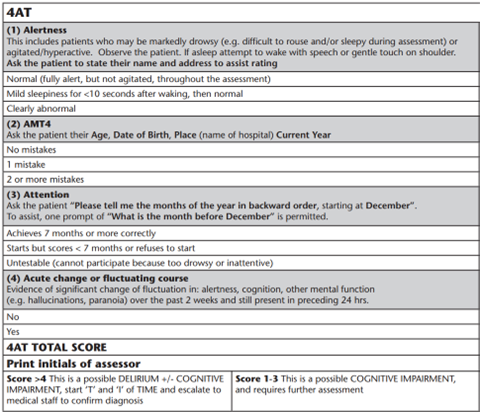
The 4AT tool is used to identify patients with probable delirium in emergency departments and acute hospital settings. Being aware of it, when visiting ward patients can be really useful.
DO to Decrease the risk of Delirium by preventing complications.
- Discuss how a Prosthesis or Orthosis could facilitate early mobilisation and reduce falls.
- Discuss how P & O interventions could reduce or manage pain.
- Discuss how P & O interventions could reduce the risk of pressure sores in tandem with increasing activity, which may help promote good hydration along with relevant nourishment.
- Consider how your communication may be less effective if the person you are treating doesn’t have their glasses or hearing aids on. Not feeling comfortable or in control of the environment could lead to feelings of isolation, which should be reduced where possible.
- Consider providing education to Carers, relatives and others on the four D’s of Delirium as you go about your daily routine
Information developed from:
Sign Guideline SIGN 157, March 2019 ISBN 978 1 909103 68 9
https://www.sign.ac.uk/our-guidelines/risk-reduction-and-management-of-delirium/
Blogs by Christine Steel, AHP Dementia Consultant, NHS Greater Glasgow and Clyde.