Could you be a Prosthetist/Orthotist? Scroll through our Human Library below to see what career paths are available.



Hi, my name is Christabelle Asoluka, and I take immense pride in being a part of the prosthetic and orthotic community here in the UK. Reflecting on my journey into this profession, I’m struck by how far I’ve come in just a few short years. Having received my training in Nigeria, I’ve had the unique privilege of gaining first-hand experience as a prosthetist/orthotist on two continents.
My commitment to this field has been driven by a genuine desire to enhance rehabilitative services for individuals grappling with various impairments, deformities, and mobility challenges.
After graduating with my bachelor’s degree in 2018, my professional journey has taken me on a diverse and exciting path. This journey has encompassed roles in the commercial sector, exploration of cutting-edge technologies, dedicated research pursuits, leadership roles, and invaluable clinical experiences, all within prosthetics and orthotics. Over the past five years, I’ve crafted my unique career trajectory to show how many things one can do in the profession.
As a newly qualified orthotist in the UK, I am currently in a graduate orthotist role. A big part of this experience has been the rare opportunity to shadow different orthotists.
So what does a day in my life look like?
Morning Commute and Clinic Preparation
Orthotist’s Role and Patient Interaction
The most rewarding aspect of being an orthotist is the opportunity to be integral to individuals’ journeys toward improved well-being. Many mistakenly confuse us with cobblers or podiatrists initially, but when patients comprehend the scope of our expertise and how we can positively impact their lives, their faces light up with hope and gratitude
I genuinely enjoy engaging with our patients and learning about their life stories. My mentor, Kristina, is exceptionally skilled in this regard. Her profound understanding of our patients’ backgrounds creates a warm and welcoming atmosphere in her clinics.
Orthotics is an intricate discipline that demands analytical thinking and rapid problem-solving abilities. Patient-centred care is at the core of our practice because an orthotic device serves no purpose if the patient does not embrace it. The profession is undeniably hands-on, and orthotists often acquire do-it-yourself skills to meet patients’ unique needs.
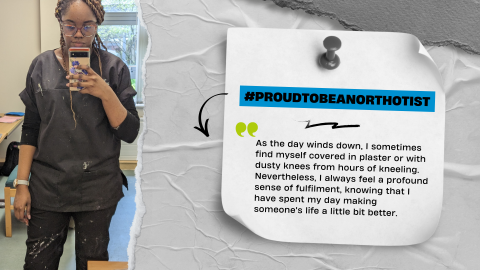
As the day winds down, I sometimes find myself covered in plaster or with dusty knees from hours of kneeling. Nevertheless, I always feel a profound sense of fulfilment, knowing that I have spent my day making someone’s life a little bit better. While the path of an orthotist isn’t always smooth, and occasionally patients may not be as appreciative as we hope, more often than not, we are showered with gratitude and thanks for the positive impact we bring to their lives.
In conclusion, the day-to-day life of a newly qualified orthotist is a diverse and rewarding experience. We bridge continents, cultures, and individual stories in our quest to improve the lives of those who rely on our expertise and care.
As we celebrate P&O Day this year, I want to take this opportunity to applaud all newly qualified prosthetists and orthotists for their hard work and dedication. I also want to express gratitude to the seasoned practitioners who have dedicated decades of their lives to this noble profession. Your commitment has paved the way for us to follow, and for that, we say thank you.
Once again, I cannot emphasize enough how deeply proud I am to be an orthotist.
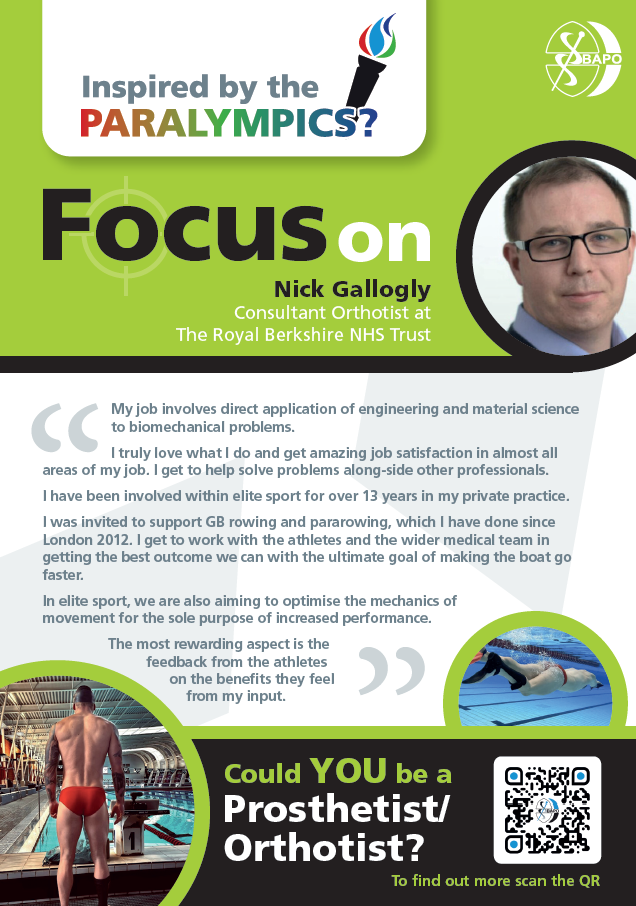
My name is Jourja Pattrik, I am a Junior Orthotist at the Royal Berks in Reading. I graduated in 2022 and have been in the job a year this month.
Every morning starts the same; I get into the office for 7am and have a brief meeting (and a cup of tea) before our first patients at 7:30. Our department provides NHS Orthotic services to patients within the Reading and wider Berkshire area. An Orthotic patient could be seeing us from a child growing into an adult or for a brief time such as an inpatient on a ward. Below is an example of what my day entails as a graduate Orthotist.
7:30– I start my first appointment, today it was a new FFO for a lady with metatarsalgia. She tells me today she has had ongoing issues with her feet for the last 10 years and feels she is always walking on pebbles. She was able to explain her symptoms in detail and her referral included all the relevant information to help me in the appointment.
We discussed her footwear and agreed to trial a modular FFO with a met dome to allow for some offloading to her metatarsals and reducing the pain. She was able to trial these today in our appointment, found immediate relief, and was very happy. We agreed to review in a few months and ensure still getting on with them.
8:00– I then have a review of an AFO for a lovely girl who was an inpatient on one of the wards. She has complex neurological conditions and due to being in a wheelchair all day is at risk of contractures. Her mum tells me today she is back home and doing well. The AFOs are still fitting well and we checked them over today. Mum tells me they are having trouble keeping her feet inside the AFO as she does not wear shoes in her wheelchair and so is able to wriggle her toes over the edges. We trialled today adding a toe strap which is able to keep the toes in place whilst she was wearing and mum was very happy. We gave a few extra straps just in case they were lost and agreed to review her with growth.
8:30– My next patient was a new FFO for a little boy with pain in his feet. He tells me is has pain in the bottom of his feet along the middle. He was able to tell me he has pain when he first walks up and sometimes after football. He tells me he also plays basketball outside of school for fun but sometimes this hurts. I was able to complete a full assessment and explain to him and his dad the presentation of his feet. We agreed to trial a pair of stock FFOs with the aim of reducing the stress/ strain on his soft tissues. I advised dad having feet that roll in a little is normal but pain and instability are not. Dad was aware and happy with this and we agreed to review with growth.
9:00– I had a new knee brace today for a man with medial osteoarthritis affecting his right knee who has been seen by orthopaedics but is not suitable for surgery. This is due to his age. He reports he is still quite young and active and so hoping to reduce his pain and stay active at the gym. He tells me he has a lot of pain in his R knee, especially at the end of the day or after the gym. We did a full assessment today and checked his ROM and laxity levels. I took some measures today and will order 2 different knee braces for his fitting appointment to ensure he finds a brace which is not only helpful and reduces pain but which he will be compliant in wearing.
9:30– I had another new FFO for a lady with previous Tibialis Posterior surgery 15+ years ago and arthritis in her L knee. She tells me today she has a lot of pain in her L medial side of her knee and pain in her medial side of the foot. She tells me in the last 6 months she has had to be less active due to the pain. Her daughter tells me she is also complaining of pain more in her feet and the knee even when just doing jobs around the house. Today she was wearing very flexible flat shoes with no fastenings, which she tells me she wears all the time or her slippers at home. I did a full assessment today of her foot and ankle and she presented with a pes planus foot type on the L with rearfoot valgus and difficulty on single leg heel rise on L. She was painful on inversion when checking ankle ROM and tender along tib post tendon tracking. We discussed today her presentation and agreed to trial a pair of insoles but also advised her on her footwear. I advised the footwear is very unsupportive and therefore an FFO needs to be in a supportive shoe and provided a footwear leaflet with the information on shoes and shoe companies who make good supportive shoes. We agreed to look at these shoes in the fitting to ensure she was happy with them and could still get them on and off herself.
10:00-My final patient of the morning was a review of a shoulder brace/new AFO. This patient I have seen before but he is now having some more intense therapy and he is able to stand now with some assistance and take a few steps forward. He is a complex patient due to his brain haemorrhage leaving him with severe weakness. After taking a full assessment of his lower limbs, I advised the patients I would like to speak to one of my colleagues before making a full decision. The patient was happy with this and so I popped out to see if one of my colleagues was free. Lucking, the clinical lead and consultant orthotist had a few moments. I was able to fully describe the patient and my proposed plan, he was then able to pop into the room and see the patient and confirm the proposed plan may be possible but we would make a few changes. We discussed with the patient who was happy with this approach and so we took a cast for his left leg and wrote a prescription for the AFO together. I will then fit this when it is back in.
11:00-I then had 4 fits of FFOs, these were for different custom orthotics which needed to be fitted and the patients were advised on breaking in and next steps. I was able to see them in quick succession that made my final appointments run very smoothly.
Then I had my lunch with my colleagues and looked at the inbox for any ward referrals. There were 2 new wards which needed to be seen urgent. My colleague saw a gentleman on the stroke ward for foot drop and due to his presentation prescribed a PLS AFO to trial and review once an outpatient. I saw a lady on the Orthopaedic ward for a complex spinal injury. She had multiple rib fractures, stable fractures to her spine but also an unstable T11 fracture. With the help of the team, she was able to be log rolled for me to but a TLSO brace in situ. She found this to be manageable to her spinal injuries and I agreed I would pop back up at the end of the week to check she was still getting on.
1:30-My first afternoon patient was another 2 fittings of FFOs from previous appointments. I was again able to fit them to the patient’s shoes and advice on breaking in and the next steps. We were also able to provide or guidelines for FFOs leaflet with the information in writing.
2:00-Finally, I saw my last patient of the day which was a new helmet. He was a 14 month old with a history of seizures, he was seen with his mum. This was my first helmet appointment without shadowing but I was able to take a full assessment and we agreed to trial a stock helmet first to see if he could tolerate this. I took measures for this and we agreed to book a fitting and a review to see how getting on after the fitting. Mum was very happy with this plan.
Wrapping up
After seeing all my patients I then have some time to catch up on my admin tasks. Finally, I gave the workshop and plaster room a quick tidy before heading home.


Each day varies for a prosthetist. You don’t always know what is coming through the door.
My day starts at 08.00 and ends at 18:00– I’m lucky to be able to work a condensed hours week – meaning I work 4 days a week (and get a 3-day weekend).
Today I came in a little early, knowing I had a patient booked for 08.00. I turned the computer on and checked what was in store for the day.
08.00 came and I collected my patient from reception and introduced myself – being relatively new to the department, many of the patients I see do not know me yet and its important to ensure they know who you are, and that you begin to build the patient/clinician relationship well from the start.
We walked around to the clinic room and the assessment commenced. The patient was having noises coming from his leg, and the socket was rubbing on his knee. I checked the residual limb and identified the area causing the rub, then took the prosthesis to workshop for the technician to check the limb over and repair anything that may be causing the noise. I adjusted the socket to reduce the pressure and then returned the prosthesis to the patient to trial. The team had done their job – the prosthesis was no longer making noises as the patient walked, and the socket was much more comfortable – a 10/10 from the patient.
Next in was a patient for casting – a new socket was needed for their arm as they had lost some weight and therefore the socket was no longer fitting well. A cast using plaster of Paris was taken to replicate their residual limb and measurements of their arm were also taken so the team can make their arm the correct shape and length. Some cleaning was needed at the end of the appointment, as plaster of Paris can be quite messy!
A brief interlude to start writing up some clinical notes and orders came next and a chance to have quick drink of water. A tap at the office door paused this as a physiotherapy colleague needed some assistance and as all AHPs aim to do, I went to help. My colleague filled me in as we walked to the gym – the patient had recently got their first limb, and having developed their walking, was beginning to struggle a little with the prosthesis set up – they were catching their toes when walking. We assessed all possible causes – was the socket too big, or too small, was the prosthesis too long, was the foot angled correctly and had the patient changed shoes? Once lots of questions had been asked and assessments completed, we found that the patient had decreased in volume of their stump, which is common in primary/new amputees. We checked the fit using stump socks and after adjustments, the patient was walking much better again, and no longer catching their toes.
Another colleague and I stopped for lunch at the same time today, and decided to sit outside for some fresh air and a chat whilst we ate. Its always helpful to be able to take a few minutes to chat through some situations, get some sun and generally check up on others to make sure they are ok through the day.
The afternoon started with a department meeting. We had some product/component demonstrations and discussions over challenging cases. Working closely with the MDT and other prosthetists helps spread learning and ensure a holistic view of cases are taken and all clinical staff are aware of any plans.
Once the meeting finished it was back to the computer to finish notes, orders and arranging some appointments whilst I waited for the last patient of the day. Unfortunately, they did not attend the appointment, and they didn’t call to let us know. The team rebooked the patient for a few weeks’ time and a letter will be sent in the post to confirm this appointment in the hope they will attend.
I find completing my admin and tying up loose ends before moving on to my plaster work allows me to focus better on the rectification needed. Following the admin, I went to the rectification room to work on the cast I took in the morning. The cast was filled with plaster and the outer shell removed so I had a copy of the residual limb that I could adjust and smooth to ensure a good fit. Details for manufacture were documented on the cast and passed through to the workshop for manufacture.
I finished my day by cleaning down my work bench and rectification area, then replying to a couple of emails before logging off and heading home.
Today was a good balance of both patient facing and MDT working. Some days can be more patient facing, others could be more meetings and courses, but every day is a learning experience and provides many opportunities to help others needing our expertise.
Every day I make a difference to those who come for appointments, be that stopping their limb making a noise so they can walk along the corridor without people looking at them curiously, reducing discomfort to make walking more comfortable or solving problems to make life and every day living easier for the patients in our care.
I get the chance to solve problems, work alongside a great team, get messy and creative with hands on skills, see new and innovative products and above all, have a positive impact on peoples lives.
I find completing my admin and tying up loose ends before moving on to my plaster work allows me to focus better on the rectification needed. Following the admin, I went to the rectification room to work on the cast I took in the morning. The cast was filled with plaster and the outer shell removed so I had a copy of the residual limb that I could adjust and smooth to ensure a good fit. Details for manufacture were documented on the cast and passed through to the workshop for manufacture.
I finished my day by cleaning down my work bench and rectification area, then replying to a couple of emails before logging off and heading home.
Today was a good balance of both patient facing and MDT working. Some days can be more patient facing, others could be more meetings and courses, but every day is a learning experience and provides many opportunities to help others needing our expertise.
Every day I make a difference to those who come for appointments, be that stopping their limb making a noise so they can walk along the corridor without people looking at them curiously, reducing discomfort to make walking more comfortable or solving problems to make life and every day living easier for the patients in our care.
I get the chance to solve problems, work alongside a great team, get messy and creative with hands on skills, see new and innovative products and above all, have a positive impact on peoples lives


Jonathan Wright MBE MBAPO
Orthotist
The global twists and turns of a career road less travelled
It wasn’t a smooth start. Moving countries when you are young has mixed blessings, as does returning to your own country when the time comes. Travel is a great educator, but education and qualifications don’t always travel well. This was overmuch the case with me.
I decided to return to England at 19 years of age, education in tatters, £25 in my pocket, one change of clothes in a small suitcase, guitar on my back and homeless (my parents having decided to remain in Africa ). Not a good position to be in.
Things rapidly worsened. Whilst attending an interview at a college on the South Coast to register for GCSEs, I was informed that due to my tax status and having been residing out of England for some years, I was classed as an “overseas student”. I would need to pay a couple of thousand pounds to study. Clearly, this was not an option and after a few hours in a local pub, building up the courage to go back to the college to further plead my case, I was still told that, the only other way to get in without charge was to work for three years, to pay tax and National Insurance and then re-apply. This I did.
During that time the challenge of finding work was only equalled by the inherent problem of where to live. The latter on occasion coming with the former, but in the main if fortunate, staying in charity hostels such as “Centre Point” in London and if not, fields or bus stations had to suffice.
Fast forward three years, it is now 1982. Having satisfied the system, attaining a few foundational and recognisable qualifications, I was successful in the job market and was employed by an Orthotics company as a Trainee Orthotist. They later went on to sponsor me on the P&O course in Paddington which, at the time, was the first of the new courses in England.
To say I struggled with this learning process was an understatement. But we were housed in hotels near the college and living and working with class mates was a truly memorable experience, resulting in several life-long friendships.
Once we qualified and went our separate ways, it was “teeth-cutting” time! I started my career in London, working in many of the inner city hospitals, gaining valuable experience in Orthotics.
After taking a senior post in Cornwall, employed by the County Council who ran the Orthotics service, which was somewhat unusual, I applied for my first job overseas.
I was fortunate enough to secure a post in a Non-Government Organisation (NGO), run by Sandy Gall, having been interviewed by the “grandfather of Orthotics”, Bill Tuck. In addition to a clinical role, I was also tasked with developing a training programme and establishing an orthotics clinic in Afghanistan. Working in such an environment is difficult to describe, there are so many extra duties and factors influencing daily routine, from language and cultural challenges to security issues and international matters concerning personal and professional arrangements.
Much of this cannot be learned from a text book!
The “University of trial and error” is the best way I can describe this learning curve.
One of the most important skills needed was the ability to communicate and negotiate with other colleagues, organisations and the military. Information and networking are essential skills needed when establishing a successful project.
Constraints often occur in such fluid situations, so you have to constantly keep your “ear to the ground”. The hard work paid off. By 1989, the clinic was successfully established in North East Afghanistan and in the same year, the training programme was judged as the best of its kind by the World Health Organisation.
Moving on to Sri Lanka, I undertook two country-wide surveys in the civil war there on behalf of another NGO, with a view to starting a P&O school. This involved negotiating with the various factions at government level and with representatives of the Liberation Tigers of Tamil Eelam. Working within the country during a time of conflict was quite different from my previous job, as it involved negotiating with both civilians and the military, collating very sensitive information in order to establish a meaningful overview of the need for P&O in the short and long-term. I became versed in the intricacies of landmine construction, placement and impact.
Extending my interest in working within conflict zones, my career took me to Cambodia, Mozambique and finally Bosnia, undertaking clinics, presenting papers on P&O, promoting new Prosthetic limb systems, developing project proposals, monitoring and evaluating projects and writing impact studies.
I became involved in the rehabilitation of service veterans and worked closely with BLESMA (the limbless veterans) charity, BCEL (British Commonwealth Ex-Service Men’s League), CAFOD (Catholic Agency for Overseas Development) and various other organisations.
My career has also lead me to work in Germany, Switzerland and New Zealand gaining an invaluable insight into P&O on an international scale, but this was interspersed with undertaking a great number of NHS clinics throughout the UK.
My clinical time has been enhanced with involvement in our professional organisations, i.e. BAPO and HCPC (Health and Care Professions Council), various National NHS Reports, such as “Darzi” and “Carter”, undertaking reviews on NHS Hospital departments and assisting commercial companies in contracting and technical training.
More recently, I have become a P&O “trailblazer”, constructing a pre-course for newly employed students prior to the inception of the programme proper, and I have also mentored students on several occasions over the years.
Over the course of my long career, I have been awarded the M.B.E for my services to disabled people and associated work internationally, the Bader Prize for commitment in my work treating war veterans and various travel sponsorships. My work has been noted in World Health Organisation reports and I have presented many papers on the treatment of refugees and war casualties both at international military and civilian conferences. I have worked in clinical, leadership, research and education roles including project development, training, monitoring and evaluation, and undertaking impact studies and logistical analyses in conflict zones.
I hope that my story shows that within our profession you can follow your own pathway. I hope I have served it well by elevating it both internationally and nationally.
In conclusion, I would like to return to the beginning of my story and thank my old guitar, which once sold, contributed funds to my decision-making pub session all those years ago, providing me with enough “Dutch Courage” to gain the all-important, albeit daunting information necessary to embark on my pathway of studies and subsequently my career in Prosthetics and Orthotics.
Some of my roles within my career:
Trainee Orthotist
Orthotist in NHS and Local Authority services
Team leader (establishing new P&O clinic in Afghanistan)
Lead Clinical trainer (developing WHO recognised P&O course in Pakistan)
Lead Author (including for two major surveys to establish a P&O school in Sri Lanka)
Freelance Orthotist and Writer (writing project reviews for P&O projects in Cambodia)
Lead presenter and project reviewer (for P&O in Mozambique and in Bosnia)
Lead P&O professional co-directing “limbs for Bosnia” in conjunction with BLESMA ((the limbless veterans charity)

Visit our Human Library for Support workers and Technicians below: