As we near the end of another remarkable year, the British Association of Prosthetics and Orthotics (BAPO) is gearing up for an exciting season of celebration, innovation, and progress across our profession.
🎉 Annual Awards & 30th Anniversary Celebration
On 21 November in Glasgow, we’ll come together for BAPO’s annual awards — a special event that also marks our 30th anniversary. With a record-breaking 205 nominations across 12 categories, we’re thrilled to see so many colleagues recognised for their outstanding contributions to prosthetics and orthotics. Congratulations and best of luck to everyone shortlisted!
That same day, we host our final conference of the year, themed “Working Together.” The programme features a packed schedule of clinical sessions and three outstanding keynote speakers. We’re proud that BAPO remains the only AHP professional body to offer fully funded member tickets — demand was overwhelming, with tickets selling out in record time!
New Guidance Publications
BAPO has recently released three new guides:
- Clinical Record Keeping, Data Protection, Confidentiality, and Consent
- Safeguarding Children and Vulnerable Adults: A Guide for Prosthetists and Orthotists
- Service Provision Guidance for Prosthetic & Orthotic Services
These resources set clear benchmarks for best practice and can be downloaded via the website.


BAPO’s Partnership Programme
We’ve relaunched our Corporate Partner scheme as the BAPO Partnership Programme, designed to strengthen collaboration with industry and charity partners. This initiative supports joint efforts to tackle the challenges facing our profession. We’re delighted to now have 21 BAPO Partners, with more set to join as the scheme develops. Together, we’ll continue to build stronger, mutually beneficial partnerships.
Education and Learning
Education remains at the heart of BAPO’s mission. We’re expanding our education offering with a series of new courses planned for 2026, including an exciting partnership with ISPO UK to deliver a comprehensive suite of online learning opportunities — more details coming soon!
A warm welcome also goes out to our first-year learners at Salford and Strathclyde University — we wish you the very best as you begin your journey into prosthetics and orthotics. BAPO has recently sent all first year learners a welcome pack with information and merchandise from some of our BAPO Partners.

Technician and Support Worker Committee
We’re pleased to announce the appointment of Bex Wilkinson as Chair and Sam Baker-Jackson as Vice-Chair of our newly renamed Technician and Support Worker Committee. This inclusive name better reflects the breadth of our workforce, and engagement has been fantastic — we now have a full, diverse, and active committee.
Meet the Prosthetics & Orthotics Career Outreach Team
Our Prosthetics and Orthotics Career Outreach Team is dedicated to inspiring, supporting, and guiding the next generation of professionals in this vital healthcare field.
We work to raise awareness of the rewarding careers available in prosthetics and orthotics, connecting students, educators, and practitioners through outreach, education, and partnership.
Our Mission
We aim to:
- Promote awareness of prosthetics and orthotics as dynamic and patient-focused professions.
- Support entry pathways and educational opportunities for aspiring clinicians and technicians.
- Collaborate with schools, universities, and employers to grow a diverse and skilled workforce.
- Showcase real-world impact through stories, innovation, and clinical excellence.
What We Do
The team delivers career talks, workshops, and mentorship opportunities across the UK — highlighting the blend of science, engineering, and compassion that defines prosthetic and orthotic practice. We also provide tailored resources for educators and career advisors to help guide students into this unique profession. The team consists of Lauryn Campbell, Career Outreach Lead and the Career Outreach Officers, Francesca Makey, Sam Baker-Jackson, Samina Khan, Manuela Mundy, and Gail Morrison.
Sustainability
BAPO recently released its Top 10 Sustainable Priorities for the prosthetics and orthotics profession. Mary Ezeuzo will be discussing these in detail during her Teatime Talk on 16 February 2026 — don’t miss it!


New Networks
We’re excited to announce the launch of several new professional networks designed to strengthen collaboration and peer support:
- Learner Network – led by Abby Bryon and Jenson Mullen
- Practice Educator Network – led by Gary Carden and Becky Stevens
These networks are open to all UK-based learners and educators, regardless of BAPO membership. For more information, please contact enquiries@bapo.com
New Roles at BAPO
We’re thrilled to welcome several new faces to key leadership roles:
- Mary Ezeuzo – Public Health and Sustainability Lead, providing updates as she completes her Public Health Fellowship.
- Lauryn Campbell – Career Outreach Lead, coordinating outreach and volunteer recruitment. (Contact: Lauryn.Campbell@BAPO.com)
- Maeve Cassidy – First BAPO Champion, leading communications, resource sharing, and peer support through a dedicated Microsoft Teams channel.
- Christabelle Asoluka – Digital Lead, supporting the integration of emerging technologies such as AI and simulation to align with the NHS 10-Year Plan.


Advocacy and Representation
BAPO continues to represent the profession at the highest levels through active engagement with:
- NHS Supply Chain, Health Improvement Scotland, and HCPC
- National policy groups, AHP Workforce Priority Setting Partnership, and NHSE education networks
- International collaboration with P&O bodies in New Zealand and Australia
We’re also working with Limb Power, BLESMA, NHS England, and NHS Supply Chain to establish both a stakeholder group and a dedicated All-Party Parliamentary Group (APPG) for prosthetics and orthotics.
In addition, our new partnership with the Lindsay Leg Club aims to enhance quality of life for people living with lower limb conditions — from leg ulcers to limb difference — through awareness, empowerment, and education.
Updated Locum Register
BAPO has updated its Locum Register to now include Private Practices, providing a central resource for anyone seeking access to prosthetic and orthotic services outside the NHS. While BAPO does not endorse individual providers, all listed professionals are HCPC-registered and current BAPO members.

Global Collaboration
We’re proud to announce an international partnership between BAPO and the Swedish Orthopedic Technical Association (SOTF). Together, we aim to strengthen prosthetic and orthotic care worldwide — recognising that global challenges demand global solutions.
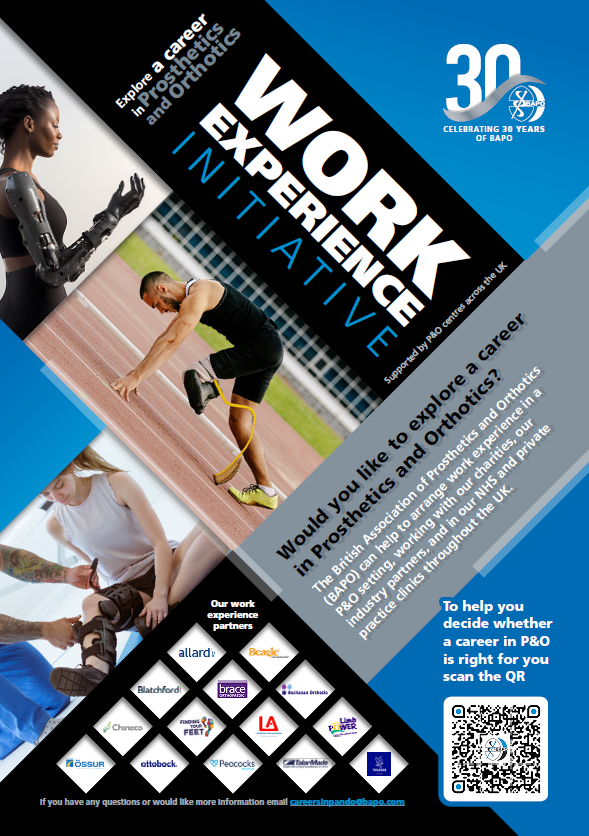
Work Experience Initiative
BAPO are thrilled to launch the Work Experience Programme for anyone interested in exploring a career in Prosthetics and Orthotics (P&O). This national initiative, co-ordinated by the British Association of Prosthetics and Orthotics (BAPO) and supported by our amazing partners, charities, and NHS P&O services, aims to give people the chance to experience first-hand the innovative, compassionate, and life-changing work that happens across our profession. Providing meaningful opportunities for people to engage with prosthetics and orthotics is crucial to supporting the future workforce pipeline. By opening our doors, we can inspire the next generation of prosthetists, orthotists, technicians, and support workers who will shape the future of P&O care.
We’re calling on our community to help spread the word! If your organisation would like to host work experience placements, we’d love to hear from you, please get in touch at careersinpando@bapo.com
Looking Ahead
As we celebrate 30 years of BAPO, we’re filled with gratitude for our members’ passion and commitment. The year ahead promises exciting opportunities for growth, collaboration, and innovation across the P&O profession.
Stay connected and informed by subscribing to the BAPO newsletter (Bottom of the page) — and here’s to an inspiring 2026!